Abstract
Eosinophils play a pivotal role in the inflammatory pathology of asthma and have been the target of new biologic treatments for patients with eosinophilic asthma. Given the central role of interleukin (IL)-5 in the eosinophil lifecycle, several therapies directed against the IL-5 pathway have been developed, including the anti-IL-5 antibodies mepolizumab and reslizumab and the IL-5 receptor α (IL-5Rα)–directed cytolytic antibody benralizumab. Eosinophil-depleting therapies represent a relatively new class of asthma treatment, and it is important to understand their long-term efficacy and safety. Eosinophils have been associated with host protection and tumor growth, raising potential concerns about the consequences of long-term therapies that deplete eosinophils. However, evidence for these associations in humans is conflicting and largely indirect or based on mouse models. Substantial prospective clinical trial and postmarketing data have accrued, providing insight into the potential risks associated with eosinophil depletion. In this review, we explore the current safety profile of eosinophil-reducing therapies, with particular attention to the potential risks of malignancies and severe infections and a focus on benralizumab. Benralizumab is an IL-5Rα–directed cytolytic monoclonal antibody that targets and efficiently depletes blood and tissue eosinophils through antibody-dependent cell-mediated cytotoxicity. Benralizumab is intended to treat patients with severe, uncontrolled asthma with eosinophilic inflammation. The integrated analyses of benralizumab safety data from the phase III SIROCCO and CALIMA trials and subsequent BORA extension trial for patients with asthma, and the phase III GALATHEA and TERRANOVA trials for patients with chronic obstructive pulmonary disease, form the principal basis for this review.
Similar content being viewed by others
Eosinophil-reducing treatments have a favorable benefit‒risk profile when used as add-on therapy for patients with severe asthma with a dominant eosinophilic phenotype. |
Concerns around potential risk of immunosuppression due to impaired eosinophil function or eosinophil depletion have been raised, primarily based on circumstantial associations and nonclinical models. |
Safety data of the eosinophil-depleting therapy benralizumab include more than 1600 patients with severe asthma, approximately 1000 of whom received benralizumab continuously for up to 2 years, and for approximately 2700 patients with chronic obstructive pulmonary disease treated for up to 1 year. |
Benralizumab was generally well-tolerated by patients, with no apparent association between treatment and increased risks of infections or malignancies. |
1 Introduction
Asthma is a highly prevalent airway disease that affects more than 339 million people worldwide, approximately 10% of whom have severe or uncontrolled asthma [1, 2]. Global Initiative for Asthma (GINA) recommendations and European Respiratory Society/American Thoracic Society (ERS/ATS) guidelines define severe asthma as requiring high-dosage inhaled corticosteroids (ICS) plus a second controller and/or systemic corticosteroids for the prevention of uncontrolled asthma or asthma that remains uncontrolled despite therapy [3, 4]. Extensive research has been conducted on the underpinning pathogenic mechanisms of severe asthma.
A successful novel treatment approach for patients with severe asthma has focused on decreasing eosinophilic inflammation. Eosinophils are enigmatic cells of the innate immune system, and defining their role is a topic of intense scrutiny and debate [5]. Eosinophils have a recognized role in the defense against helminth parasitic infections and contribute to the pathology of a variety of diseases, including conditions involving T-helper type 2 (Th2) inflammation [6]. Studies have indicated that approximately 50% of patients with mild to moderate asthma have airway eosinophilia and that elevated blood eosinophil counts are associated with greater disease severity [7,8,9,10,11]. Sputum and blood eosinophil counts are also important factors for predicting asthma exacerbations [12, 13]. Eosinophils accumulate in patients’ lungs and play a role in inflammation and tissue damage through the release of cytotoxic products contained in their granules [14]. Eosinophils promote Th2 inflammation through a wide range of surface molecules and receptors, including antigen presentation and cytokine-mediated modulation of local lymphocytes [5, 6]. There is also strong evidence that eosinophils contribute to airway remodeling in asthma through the release of several growth factors and fibrogenic mediators [15]. Recent studies in mice have demonstrated that, in addition to their proinflammatory roles, eosinophils may also contribute to homeostatic functions, including immunomodulation [16, 17]. These studies support the “LIAR hypothesis” put forth by Lee et al. [18], which proposes that accumulating tissue eosinophils are actually regulators of local immunity and/or remodeling/repair in both health and disease.
Interleukin (IL)-5, a homodimer cytokine, is one of the main eosinophil modulators and acts at several functional levels and time points during the eosinophil lifecycle. IL-5 exerts its effects on proliferation, differentiation, and maturation via receptors that comprise an IL-5–specific α- and common β-subunit [19]. The IL-5 receptor α (IL-5Rα) chain is highly expressed in human eosinophils and, to a lesser extent, by basophils and mast cells [20]. IL-5 contributes to the egress of eosinophil-committed progenitors from the marrow to the intravascular compartment [21] and attracts eosinophils and primes them for activation [22]. IL-5 has also been demonstrated to prolong the survival of eosinophils in submucosa [22].
Given the central role of IL-5 in the eosinophil life cycle, several therapies targeting the IL-5 pathway have been developed with the aim of decreasing eosinophilic inflammation and associated tissue damage for patients with asthma. Two monoclonal antibody treatments inhibiting IL-5—mepolizumab and reslizumab—have been approved in the USA, Canada, Europe, and Japan for the treatment of patients with severe asthma with an eosinophilic phenotype, and mepolizumab is available in more than 20 other markets as well [23,24,25,26]. Both mepolizumab and reslizumab directly bind to circulating IL-5 and reduce eosinophil counts via inhibition of IL-5 signaling. By contrast, benralizumab is an IL-5Rα–directed cytolytic monoclonal antibody that induces rapid and nearly complete eosinophil depletion via enhanced antibody-dependent cell-mediated cytotoxicity [27, 28]. Benralizumab is approved in the USA, Europe, Japan, and many other countries for the treatment of patients with severe asthma and an eosinophilic phenotype.
Benralizumab has been explored for the treatment of diseases other than asthma with prominent tissue eosinophilia, including hypereosinophilic syndromes (HES) and chronic obstructive pulmonary disease (COPD). HES are rare and often debilitating chronic inflammatory disorders characterized by blood and tissue eosinophilia, with associated eosinophil-mediated organ damage and/or dysfunction [20]. In a phase II trial, benralizumab reduced absolute eosinophil counts compared with placebo for patients with platelet-derived growth factor receptor A (PDGFRA)-negative HES [29]. Sustained clinical and hematologic responses were observed for most patients during the open-label phase of the trial. COPD is characterized by persistent respiratory symptoms and airflow limitation due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases [30]. It is estimated that up to 40% of patients with COPD have eosinophilic inflammation [31, 32], and approximately 20% of exacerbations have been identified as eosinophilic exacerbations [33,34,35]. The role of eosinophils in COPD may differ notably from that in asthma and other diseases [36].
Because eosinophil-lowering therapies represent a new class of compounds to treat asthma and potentially other diseases associated with eosinophilic inflammation, it is important to examine their long-term efficacy and safety. Eosinophils have traditionally been associated with host protection against helminthic parasitic infections. However, recent studies have demonstrated a contrasting role for eosinophils in supporting the growth and protection of parasites [37]. Innate eosinophil functions have also been implicated in the immune response to viruses in animal models—findings that may have implications for humans [38]. It is also well-established that eosinophils infiltrate a variety of solid and hematologic tumors, playing both pro- and antitumorigenic roles [39]. Consequently, it is important to understand whether eosinophil depletion or reduction could incur potential safety concerns for patients. In this review, we explored the safety of the eosinophil-depleting therapy benralizumab and the potential risks associated with eosinophil depletion, with particular focus on malignancies and severe infections.
2 Epidemiology of Malignancies and Infections in Patients with Asthma
Asthma is characterized by chronic lung inflammation, with airway hyperreactivity, excessive mucous formation, and respiratory obstruction [2]. Patients with asthma have a greater risk of developing a range of other health conditions than does the general population [3]. Before focusing on eosinophils, we provide a summary of the published evidence and the potential underpinning pathophysiology by which patients with severe asthma may be more susceptible than patients without asthma to cancers and infections. A similar discussion on the epidemiology of malignancies and infections in patients with COPD and other eosinophilic disorders for which anti-eosinophil biologics are being investigated is beyond the scope of this paper. However, clinical safety data for benralizumab in COPD and HES are briefly reviewed in Sects. 4.2 and 4.3 to provide a holistic view of its safety profile.
2.1 Malignancies in Patients with Asthma
While inflammation can play a beneficial role in repairing injured tissues, chronic inflammation has been associated with the development and malignant progression of many types of cancers [40]. Epidemiologic and clinical studies have reported that ≥ 20% of all cancers begin as a direct consequence of chronic inflammatory disease [41, 42]. The unregulated production of growth factors and oxygen species has been demonstrated to result in permanent genetic alterations and tumor initiation. Inflammatory mediators also play a role in tumor promotion, malignant conversion, and metastatic dissemination by acting directly on cancer cells and the tumor microenvironment [40, 42].
Given the important role of chronic inflammation in cancer development, a link between inflammatory conditions such as asthma and rates of malignancies has been investigated. Several studies have suggested a significant association between asthma and the risk of developing lung cancer. Finnish [43] and Swedish [44] patients with asthma demonstrated an increased risk of lung cancer, with a marginally greater standard incidence ratio reported for female (1.66 and 1.78, respectively) than for male (1.32 and 1.51, respectively) patients. A meta-analysis of 1.6 million patients with asthma across 18 studies reported a significant association between asthma and an increased overall risk of lung cancer [45]. Investigations into a correlation between asthma and lung cancer are often confounded by tobacco smoking. However, an increased risk of lung cancer has been reported to be maintained following adjustments for smoking (odds ratio [OR] 1.35; 95% confidence interval [CI] 1.15–1.59) [46] and is also evident for nonsmoking patients with asthma (OR 1.28; 95% CI 1.10–1.50) [45].
The possibility that asthma may be associated with greater general rates of cancer has also been explored. Patients with asthma have been reported to have elevated risks of colon and rectal cancers [43], and limited data suggest an inverse association between history of allergy and cancer-related mortality [47]. However, in another study, asthma was not associated with an overall greater risk of cancer, and the risk of non-smoking–related cancer was slightly reduced for patients with asthma [46]. Given the limited data and contradictory findings, it is unclear whether patients with asthma are at greater risk of cancers other than lung cancer.
2.2 Infections in Patients with Asthma
The presence of asthma can influence patients’ susceptibility to infections [48]. This increased risk of infection is, in general, viewed as secondary to airway inflammation, particularly for patients with severe asthma. However, some evidence suggests that ICS may also be associated with an increased risk of respiratory tract infection in patients with asthma [49]. It has also been suggested that, in some cases, underlying immune dysfunction may be a phenotypical or clinical feature of asthma [48]. This is in light of findings that the risks of pertussis [50], Streptococcus pyogenes upper respiratory tract infection (URTI) [51], and Herpes zoster [52] are independent of asthma control status or severity. It has been reported that rhinovirus infection, the severity of which might relate to impaired immune function, is a risk factor for bacteria, such as Streptococcus pneumoniae, for patients with asthma [53]. Thus, some clinicians have suggested making vaccination (e.g., pneumococcal) a part of all adult asthma treatment plans and not limiting its use to older patient groups [48, 54, 55].
3 The Role of Eosinophils in Malignancies and Infections
3.1 Eosinophils in Malignancies
It is well-established that eosinophils infiltrate a variety of solid and hematologic tumors. However, the contradictory pro- versus antitumorigenic roles of eosinophils in cancer have been difficult to reconcile [56]. Evaluation of current evidence regarding eosinophil function in infectious disease and tumor biology will help address potential concerns regarding the therapeutic ablation of eosinophils for patients with asthma. The principal question of interest, based primarily on retrospective epidemiologic studies or animal models, is whether the absence of eosinophils alters the natural history of tumor progression. Whether eosinophil infiltration is associated with a favorable or unfavorable prognosis remains controversial and appears to depend on a range of factors, mainly the type of cancer [39]. An association between eosinophil infiltration and prolonged survival has been reported in biopsies for patients with rectal/colorectal cancer [57, 58], oral squamous cell carcinoma [59], pulmonary adenocarcinoma [39], and nasopharyngeal carcinoma [60]. Similarly, elevated serum eosinophil counts during prostate cancer therapy were associated with a survival benefit [61]. By contrast, eosinophil infiltration is associated with poor prognosis in some, but not all, patients with Hodgkin lymphoma [62,63,64], multiple myeloma [65], or cervical cancer [66, 67]. Associations between prolonged survival and low eosinophilic markers in microarray biopsy data for patients with lung cancer have indicated that eosinophils may also contribute to tumorigenesis in the lung [68].
Although eosinophil infiltration of tumors is common, the causes and consequences of eosinophil recruitment and accumulation for tumorigenesis are unclear. Several lines of evidence have suggested that tumor-associated eosinophilia may be an epiphenomenon related to elaboration of eosinophil-active factors or tumor stage, without clear influence on the natural history of the disease [57, 69]. Notably, patients lacking eosinophils, in the setting of immunodeficiency or as a consequence of immunoglobulin G-mediated eosinophil precursor destruction, do not display any distinguishing abnormalities related to eosinophil reduction [70,71,72]. Prior to the advent of biologics, oral corticosteroids (OCS), which also deplete eosinophils [73], were used for decades without any reports of increased malignancy rates [74, 75].
Several murine studies have provided conflicting results on the role of eosinophils in cancer. First, there have been no reports of a distinctive syndrome or health failure across several eosinophil-deficient mice strains under ordinary laboratory conditions [69, 76,77,78]. While some studies have reported that eosinophils have no tumoricidal activity [79, 80], preclinical models of inducible or transplantable tumors have suggested a role for eosinophils in tumor regression and an increase in tumor incidence in the absence of eosinophils [81,82,83]. Other preclinical studies have examined the potential mechanisms linking eosinophils to cancer, with a particular focus on IL-5. While initial studies reported that IL-5 did not alter lung tumor formation [84], subsequent reports noted that IL-5 enhanced adenocarcinoma-induced malignant pleural effusion [85] and facilitated metastatic colonization through recruitment of sentinel eosinophils in the distal lung microenvironment [86]. IL-5–producing cells may also play a role in tumor surveillance through lung eosinophils [87]. The direct relevance of findings in mice to patient risk during treatment with eosinophil-lowering therapies remains unclear. This is particularly relevant because benralizumab does not bind to murine IL-5Rα [88]. Benralizumab does bind to IL-5Rα on human and cynomolgus monkey eosinophils with similar affinities, suggesting this is a more suitable model for benralizumab studies [89]. Repeat-dosing studies for up to 39 weeks in cynomolgus monkeys indicated no adverse changes in organ weights or any histologic findings suggestive of preneoplastic lesions [89].
There is no evidence that persistently low or absent eosinophil counts, as a result of pharmacological targeting, genetic manipulation, or a pathologic process, result in an increased incidence of cancer. The incidence of treatment-emergent malignant neoplasms for the anti‒IL-5 treatment arms of the controlled asthma exacerbation trials for mepolizumab and reslizumab was < 1% and generally similar to that for placebo for exposures up to 1 year [90, 91]. The published incidence of malignancy over extended exposure times for these same modalities was 6/347 (2%) for open-label mepolizumab (up to 4.5 years) and 12/1051 (1.1%) for reslizumab (up to 2 years) [92, 93]. Similar results were observed for benralizumab in patients with severe asthma during the approximately 1-year placebo-controlled and 56-week extended treatment periods (4/1663 [0.24%] and 12/1576 [0.8%], respectively) [94,95,96]. The incidence of malignancy for patients continuously exposed to benralizumab from the start of the controlled treatment period through the end of the extension period (up to 2 years) was 8/1030 (0.8%). The incidence for patients with any benralizumab exposure (including patients previously treated with placebo) during this period was 17/1655 (1%). The results for benralizumab are detailed in Section 4.1.3.
3.2 Eosinophils in Infections
3.2.1 Viral and Microbial Infection
There is increasing evidence that eosinophils may play a role in protecting against bacterial and viral pathogens. Nonclinical data support that eosinophils may be activated by, and have the ability to kill, certain bacteria, and eosinopenia has been described as a feature of modeled, acute bacterial infections [5, 97, 98]. In patients, an inverse relationship between bacterial load and peripheral blood eosinophils has been reported [99, 100], and eosinopenia may predict a bacterial etiology for patients with sepsis [101]. Eosinophil degranulation products have been detected in respiratory secretions from patients during respiratory syncytial viral (RSV) infections [102], and eosinophil degranulation was associated with a more favorable outcome in mice infected with pneumonia virus of mice (PVM), a respiratory virus infection in mice similar to human RSV [103]. Antiviral activity of eosinophils has also been demonstrated in mice for other respiratory viruses, including influenza, parainfluenza, and HIV [104, 105]. However, the immunopathogenic mechanisms remain to be elucidated [106].
3.2.2 Helminth Infection
Eosinophilia is a common feature of the host response to helminth infection. Traditionally, eosinophils are viewed as a host defender and have been shown to have toxic effects on various larval worm forms in vitro [107, 108]. However, recent studies in animal models have demonstrated that eosinophils can have detrimental effects on the host depending on the parasite species, infection location, and whether the infection is primary or secondary [37]. In fact, eosinophils have been observed to support the growth and protection of some parasites [109, 110], particularly in primary infection of extraintestinal sites, in which eosinophils promote delivery of essential host resources to the parasite, which then prevents a toxic immune response that causes larval destruction [37]. Together, these data underline the role of eosinophils in generating both protection and pathology against helminth diseases.
3.3 Resident/Regulatory Eosinophils and Role for Homeostasis
Studies in mice have demonstrated that, in addition to the classic proinflammatory and antiparasitic roles of eosinophils, they may also contribute to homeostatic functions, including immunomodulation. Mainly in murine studies, these so-called resident eosinophils have been reported to regulate glucose concentrations in adipose tissue [16] and to influence microbiotic content and mucus development in the small intestine [17, 111]. Reports in human tissues have been more variable. Greater numbers of eosinophils have been preliminarily described in adipose tissue samples obtained from lean versus obese humans [112]. In addition, published evidence for a resident eosinophil population in the human gut is quite sparse except for the detection of eosinophil degranulation products in biopsy specimens from ostensibly healthy human jejunum [113].
Lung-residing eosinophils (rEOS) with characteristics distinct from those of inflammatory eosinophils have also been identified in mice, in which they have been observed to have an immunoregulatory function capable of restricting adaptive immune responses [114]. These data suggest that, in healthy mice, a population of resident eosinophils suppresses maturation of antigen-loaded dendritic cells and maintains homeostatic Th2 responses in the lung tissues. Interestingly, despite expressing IL-5R, the numbers of murine rEOS did not meaningfully change in response to IL-5 inhibition by IL-5–neutralizing antibodies [114], suggesting that their homeostatic role may not be perturbed by anti–IL-5 therapies. However, this conclusion conflicts with other results from the same study in which isolates of the same rEOS displayed typical downstream responses when exposed to IL-5 in vitro (i.e., ERK phosphorylation and viability enhancement). Since tissue eosinophil functions and activation state are largely a product of their microenvironment, and anti‒IL-5 antibody treatment, even at high dosages, does not eliminate airway eosinophilia in patients with asthma, an alternative explanation may be that these cells are being maintained by other locally active eosinophil-viability-enhancing factors [115]. In contrast, the mechanism of action of benralizumab does not rely on cytokine neutralization, which is the likely explanation for the observed near-complete depletion of eosinophils in sputum and inflamed tissue and other tissues [29, 116, 117]. The increased appreciation that the eosinophil is a product of its environment casts doubt on whether any conclusions can be drawn at all when the expression of surface markers is compared between eosinophils from the healthy lung parenchyma and those derived from asthmatic sputum [114].
More recently, intravital images of fluorescently labeled eosinophils in the murine lung in both the basal and allergen-challenged state have been published [118]. Within the limits of the technique, transient eosinophil retention in the lung was observed in the basal state, with cells rapidly detaching and re-entering the blood flow and having certain morphologic features consistent with a “patrolling” function.
The homeostatic role of eosinophils raises potential concerns about the consequences of therapeutically ablating eosinophils in humans. However, these data have been derived from murine studies, and the translational significance remains unknown. To date, there is no direct clinical evidence to support detrimental consequences of eosinophil depletion in humans.
4 Benralizumab Safety
Regarding the estimated cumulative exposure of clinical trial patients to benralizumab, approximately 11,377 patients and/or healthy volunteers have been enrolled into the clinical development program, of whom approximately 8088 have received benralizumab [119]. The safety profile of benralizumab for its approved asthma indication is the primary focus of the following discussion, with the inclusion of safety results for other indications in development for additional context.
4.1 Asthma
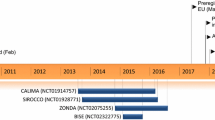
4.1.1 Integrated Analyses of SIROCCO/CALIMA and BORA
The overall placebo-controlled and extended safety profiles for benralizumab for patients aged ≥ 12 years with severe asthma, elevated blood eosinophil counts, and requiring high-dosage ICS/long-acting β2-agonist with or without other controllers have been previously published and are summarized here [94,95,96, 120]. In SIROCCO and CALIMA, two randomized, placebo-controlled phase III trials in severe asthma, patients received benralizumab 30 mg every 4 weeks (Q4W) or every 8 weeks (Q8W; first three doses Q4W) or placebo for 48 weeks (SIROCCO) or 56 weeks (CALIMA) [94, 95]. In the randomized, double-blind, parallel-group, phase III BORA extension study, patients who had completed the SIROCCO or CALIMA trials remained on subcutaneous benralizumab 30 mg Q4W or Q8W. Patients who had received placebo in those trials were rerandomized to benralizumab 30 mg either Q4W or Q8W (first three doses Q4W). Treatment in BORA was for 56 weeks for adult patients (aged ≥ 18 years) and 108 weeks for adolescent patients (aged 12–17 years) [96, 120].
Here, we present additional details from the safety analyses of these studies and their respective integrations, particularly as they pertain to the potential risk of adverse events (AE) related to eosinophil lowering, including infection/infestation and malignancy events. Table 1 summarizes the principal, sponsored data sources for this review and includes the safety assessments for the pooled SIROCCO/CALIMA studies (1663 patients receiving benralizumab [Q4W and Q8W dosing combined] and 847 patients receiving placebo) and for the 1576 patients from the SIROCCO/CALIMA studies (both benralizumab-treated and placebo-treated patients) that formed the basis for the main analysis at 56 weeks in the BORA extension study [96]. Pooling of data was possible because of similarities in study design and patient population. The principal supportive analysis for this review was the recently published integration of patients who received benralizumab in SIROCCO/CALIMA and continued into the BORA extension study, thus providing continuous benralizumab exposure for 1030 patients for up to 2 years [120]. An additional supportive analysis of patients who received benralizumab in SIROCCO/CALIMA or in BORA gives insight into patients with any exposure to benralizumab, continuous or noncontinuous, for 2 years (n = 1655; not tabulated).
For the analysis of overall AEs, we assessed all patients from the SIROCCO [29] and CALIMA [95] predecessor trials who received at least one dose of study treatment (benralizumab, n = 1663; placebo, n = 847). The frequency of overall and serious AEs during SIROCCO or CALIMA was reported by similar percentages of patients receiving benralizumab (73.7 and 11.5%) and placebo (78.0 and 14.0%) (Table 1). Most AEs were mild to moderate. The percentage of AEs leading to treatment discontinuation was greater for benralizumab than placebo (2.2 vs. 0.9%), and there were no apparent trends of types of AEs leading to discontinuation. The most frequent types of AEs (≥ 3%) in benralizumab- and placebo-treated patients in the predecessor SIROCCO/CALIMA studies are given in Table 2 and were consistent with those that would be expected in a predominantly adult population with severe asthma. Overall, add-on treatment with benralizumab was generally well-tolerated by patients with severe asthma treated during these approximately year-long asthma exacerbation studies, with overall AE types and frequencies similar to those with placebo.
A detailed internal peer review panel assessment of data from the phase III asthma exacerbation studies, pertinent information from other elements of the development program (e.g., nonclinical information), and information from outside the benralizumab development program (e.g., data from the literature and postmarketing AE reporting) indicated that several AEs are considered to have a reasonable possibility of having a causal association with benralizumab. These AEs include pharyngitis, hypersensitivity reactions, anaphylactic reaction, headache, pyrexia, and injection-site reactions and are included in the current US FDA-approved labeling and European Medicines Agency-approved labeling for benralizumab for asthma [121, 122].
The BORA study extended benralizumab treatment for patients who completed SIROCCO or CALIMA for an additional 56 weeks (adult patients) or 108 weeks (adolescent patients). The results for 1576 adult and adolescent patients (truncated at 56 weeks) have been published. The follow-on results for year 2 for adolescent patients are currently pending [96]. Patients in BORA continued to receive benralizumab Q4W or Q8W according to their treatment assignments in the predecessor studies. Patients who had received placebo were randomized to benralizumab Q4W or Q8W. The full analysis set excluded patients who, during BORA, transitioned into MELTEMI (NCT02808819), a subsequent separate open-label, 130-week safety extension study.
The results for the BORA study are presented in Table 1. The percentage of patients who had any AE (including any serious AE) was similar between SIROCCO or CALIMA and BORA, as was the percentage of patients who had an AE that led to treatment discontinuation (Table 1). The AE types and frequencies between the previous benralizumab and previous placebo groups were similar, with the most commonly occurring AEs for any group being viral URTI and worsening asthma (data not shown) [96]. The most commonly occurring AEs (≥ 3%) for BORA patients continuously treated with benralizumab since the start of SIROCCO/CALIMA were similar to those reported during the predecessor studies (Table 3); slight differences in preferred terminology are primarily a result of differences in the Medical Dictionary for Regulatory Activities (MedDRA®) version used at the time of study completion. No new safety signals were detected in previous SIROCCO/CALIMA patients after an additional 56 weeks of benralizumab exposure as part of the BORA extension study. Of note, reductions in asthma exacerbation rates and improvements in forced expiratory volume in 1 s (FEV1), asthma control, and disease-specific quality-of-life measures were sustained, without diminution, over the integrated 2-year observation period [120]. Peripheral blood eosinophil counts gradually returned toward baseline numbers after cessation of benralizumab treatment [96].
4.1.2 Infections and Infestations
The frequencies of overall, serious, and discontinuation adverse infection/infestation events in the pooled SIROCCO/CALIMA trials were similar between benralizumab- and placebo-treated patients: 857/1663 (52%) and 466/847 (55%), 30/1663 (1.8%) and 19/847 (2.2%), and 2/1663 (0.1%) and 0/847 (0%), respectively [94, 95]. Similar frequencies were observed during the BORA extension study: 756/1576 (48%), 33/1576 (2.1%), and 1/1576 (< 0.1%), respectively [96]. The two infection AEs that resulted in discontinuation of benralizumab during the SIROCCO/CALIMA controlled treatment period were the nonserious events chronic pyelonephritis and nasopharyngitis. The discontinuation due to an infection AE during the BORA extension was related to pulmonary sepsis. Of note, the frequencies of overall and common infection/infestation AEs in the subset of BORA patients continuously treated with benralizumab from the start of SIROCCO/CALIMA were similar to those observed in the predecessor studies (Table 4) [120]. No helminth infections were reported during the SIROCCO/CALIMA studies or during the BORA extension. It should be noted that such infections are uncommon in countries where IL-5–targeted therapies have generally been studied; however, the safety results for CALIMA/SIROCCO are based on results from 447 global sites, including representation beyond North America and Europe (Argentina, n = 269; Brazil, n = 36; Chile, n = 31; Peru, n = 97; Philippines, n = 61; South Africa, n = 26; and Vietnam, n = 15). Herpes zoster, which has been reported as an AE associated with certain anti‒IL-5 therapies [25], was observed in similar percentages of patients in SIROCCO/CALIMA (0.5% for both placebo and benralizumab) and the integrated treatment period (≤ 2 years) (0.6%) (Table 4). No predisposition to other opportunistic infections was evident based on these data. In summary, the overall incidence and type of infection/infestation AEs during the SIROCCO/CALIMA trials were similar between benralizumab- and placebo-treated patients and remained stable through the extended treatment period.
4.1.3 Malignancies
Malignancy AEs were assessed by an independent safety event adjudication committee (SEAC) throughout the benralizumab phase III asthma program. Only patients with an event determined by the SEAC as meeting the established criteria for a malignancy were tabulated. In contrast to the overall AE summaries, this included events reported during both the on-treatment and the post-treatment periods. Five patients reported new malignancies during the SIROCCO and CALIMA asthma exacerbation studies (four [0.2%] with benralizumab, one [0.1%] with placebo) (Table 5). A total of 12/1576 (0.8%) patients reported new malignancies during the BORA extension, which included events reported during both the on-treatment and the post-treatment periods as assessed by SEAC. Of these 12 patients, eight (0.5%) were previously treated with benralizumab in the predecessor studies and four (0.25%) were previously treated with placebo. One additional patient was diagnosed with prostate cancer prior to treatment in the CALIMA trial (in the placebo group) and did not reveal the diagnosis until after randomization to Q8W benralizumab treatment in BORA. This event was adjudicated by the malignancy subcommittee as a new malignancy but is not included in Table 5. Taken together, there were 17 malignancies as determined by SEAC during the on-treatment or post-treatment periods of SIROCCO/CALIMA or BORA, irrespective of the continuity of exposure to benralizumab. Therefore, the overall incidence of malignant neoplasms AEs in benralizumab-treated patients during the SIROCCO/CALIMA studies and the BORA extension was low (< 1%), with no apparent trends in organs or tissue types affected.
4.1.4 Comparisons with the ZONDA Oral Corticosteroid-Reduction Trial
The 28-week, phase III ZONDA trial in OCS-dependent asthma patients also evaluated benralizumab 30 mg (Q4W or Q8W [first three doses Q4W]) versus placebo for patients with severe asthma, and the primary endpoint was benralizumab’s OCS-sparing effect [117]. Benralizumab and placebo were associated with similar patterns of AEs, mostly consisting of nasopharyngitis, asthma worsening, and bronchitis. The only notable infection/infestation AE in the ZONDA trial was URTI, which was reported in similar percentages of patients who received placebo (5%) and benralizumab (6%, Q4W; 7%, Q8W). Overall, results from the ZONDA trial did not change the characterization of the potential risks associated with benralizumab beyond what was concluded from the phase III asthma exacerbation studies.
The 28-week benralizumab treatment data from ZONDA were integrated with data from the 56-week phase III BORA safety extension study [123]. The 1.5-year integrated analysis demonstrated that safety from ZONDA was maintained with further follow-up, and safety results were consistent with published data with no unexpected AEs reported. Of note, the significant OCS reductions achieved during ZONDA [117] were maintained during the 56-week BORA extension [123]. No helminth infections or malignancies were reported for predecessor ZONDA patients. The most common serious infections for patients receiving benralizumab were lower respiratory tract infection, pneumonia, and bacterial urinary tract infection (n = 1 each).
4.1.5 Postmarketing Surveillance in Asthma
Currently, the cumulative worldwide, post-approval patient exposure to benralizumab since launch is estimated to be 36,680 patient-years [119]. During the most recent reporting period, the most commonly reported serious infection was pneumonia (17 events). In total, 17 cases of spontaneous malignancies were reported, with breast recurrent (three events) and lung neoplasm malignant (two events) being the most frequent. A limitation of postmarketing data is their dependence on continual spontaneous reporting, which may not include all current, relevant events. The data received during the most recent reporting period, combined with analyses of the cumulative efficacy and safety data available, do not indicate a change in the positive benefit–risk balance of benralizumab.
4.2 Chronic Obstructive Pulmonary Disease (COPD)
The efficacy and safety of three dosages of benralizumab for the prevention of exacerbations for patients with moderate to very severe COPD has recently been explored in two randomized, placebo-controlled phase III trials, GALATHEA (benralizumab 30 and 100 mg Q8W vs. placebo) and TERRANOVA (benralizumab 10, 30, and 100 mg Q8W vs. placebo) [124]. GALATHEA and TERRANOVA offer insight into the safety of benralizumab in large, 56-week phase III trials, including a greater dosage of 100 mg Q8W and a different patient population. To provide a more detailed understanding of benralizumab’s safety profile, we conducted an integrated safety analysis of patients in the GALATHEA and TERRANOVA trials.
Across GALATHEA and TERRANOVA, a total of 2792 patients received benralizumab (10 mg, n = 561; 30 mg, n = 1117; 100 mg, n = 1114), with a mean treatment duration of 358.6 days compared with 360.8 days for placebo (n = 1118). AE types and frequencies were similar between benralizumab and placebo groups, and the most common AEs were related to COPD or respiratory conditions (Table 6). Several infection-related AEs and serious AEs were reported in GALATHEA and TERRANOVA, with similar frequencies between the benralizumab and placebo groups (Table 7).
As for the asthma development program, reports of malignancies were adjudicated by an independent SEAC. The frequencies of adjudicated malignancies were low in the benralizumab (10 mg, 6/561 [1.1%]; 30 mg, 20/1117 [1.8]; 100 mg, 22/1114 [2.0%], and 48/2792 [1.7%] for total benralizumab) and placebo arms (24/1118 [2.1%]). The types of malignancies were scattered across multiple system organ classes and representative of tissue types that would not be unexpected in this population, with the most commonly reported preferred terms (more than two patients) for the total benralizumab group being prostate cancer (six [0.2%]), basal cell carcinoma (four [0.1%]), lung neoplasm malignant (four [0.1%]), and pancreatic carcinoma (three [0.1%]) (see the electronic supplementary material). In summary, the types and frequencies of AEs reported as part of the phase III development program in COPD to date were similar in the benralizumab and placebo groups. There was no evidence of increased risks of infection or malignancy for patients with moderate to very severe COPD treated with benralizumab at dosages up to 100 mg Q8W over a period of 52 weeks.
4.3 Conditions Other Than Asthma and COPD
Anti–IL-5Rα therapy has been explored in diseases other than asthma with prominent tissue eosinophilia, including HES and immune responses following vaccination. In a 12-week phase II trial of 20 patients, benralizumab was demonstrated to reduce absolute eosinophil counts compared with placebo for patients with PDGFRA-negative HES [29]. The most common drug-related AEs—headache and elevated lactate dehydrogenase concentration—occurred for 32% of patients after the first dose of benralizumab and resolved within 48 h for all patients. Other AEs occurred with similar frequency in the two groups, including URTI. The only serious AE (hypotension) occurred in a patient receiving placebo, and there were no reports of helminth infections or Herpes zoster.
4.4 Potential Effects on Other Immune or Homeostatic Functions in Humans
Because eosinophils have been shown to have antigen-presenting functionality, at least in vitro [125], the possibility that benralizumab may modify immune system function following seasonal influenza vaccination was investigated [126]. The phase IIIb ALIZE trial evaluated benralizumab 30 mg at weeks 0, 4, and 8, plus tetravalent influenza vaccination at week 8 for 103 patients with moderate or severe asthma. Benralizumab did not impair the antibody response to seasonal influenza vaccination (assessed at week 12), and the number of patients with AEs was similar in the benralizumab and placebo groups. The most common AEs (≥ 3%) included asthma, headache, nasopharyngitis, oropharyngeal pain, viral gastroenteritis, and URTI. These results suggest that eosinophil depletion by benralizumab does not impair vaccine immune response, supporting the notion that benralizumab may not increase risk of infection. Further, indirect evidence for a lack of effect of eosinophil lowering on the humoral immune system comes from the observation that total immunoglobulin concentrations were not different for patients receiving benralizumab compared with those receiving placebo in the CALIMA and SIROCCO trials [127].
Recent observations in experimental mouse models suggesting a role for eosinophils in certain homeostatic functions such as fat and glucose metabolism naturally raise questions regarding possible effects in humans treated with eosinophil-lowering agents [16, 17]. We are not aware of any reports of disturbances in metabolic function in humans as a result of targeted, eosinophil-lowering therapies in the literature. The scope of the sponsored benralizumab database is inadequate to resolve these issues definitively. However, currently available assessments do not support a critical role for eosinophils in these homeostatic functions. No clinically important shifts or changes in hematology or chemistry in the integrated safety analysis of the SIROCCO and CALIMA registration trials were observed, and there have been no clinically important shifts in vital signs or electrocardiograms. No meaningful change in body mass index was observed in SIROCCO/CALIMA patients treated with benralizumab over the treatment period compared with placebo [127]. In addition, the frequencies of AEs related to diabetes diagnoses, glucose intolerance or hyperglycemia, or reports of “weight increased” for benralizumab-treated patients were low (< 1%) during both the predecessor and the extended (weeks 1‒56) treatment periods in the 1030 continuously exposed patients in the integration analysis (up to 2 years).
4.5 Pregnancy
Monoclonal antibodies such as benralizumab are transported across the placenta during the third trimester of pregnancy, and any potential fetal effects are likely to be greater during the third trimester. A prenatal and postnatal development study reported no evidence of fetal harm following intravenous administration of benralizumab in cynomolgus monkeys at exposures up to 310-fold the maximum recommended subcutaneous human dosage of 30 mg [121]. No AEs related to fetal or neonatal growth were observed up to 6.5 months after birth, despite suppressed eosinophil counts with gradual recovery by 6 months postpartum in most infant monkeys. A postmarketing surveillance study (NCT03794999) investigating pregnancy and infant outcomes for women with asthma exposed to benralizumab at any point during pregnancy is currently recruiting. In a long-term safety trial of mepolizumab for HES, one patient became pregnant twice during the study. The first pregnancy was electively terminated, and the second resulted in the birth of a healthy neonate [128].
5 Discussion
Eosinophil-reducing therapies that have been approved for the treatment of severe asthma include benralizumab and the anti–IL-5 monoclonal antibodies mepolizumab and reslizumab. The benefit‒risk profile of IL-5– and IL-5Rα–targeted therapies has been periodically reviewed both in the scientific exchange and as part of regular regulatory updates for the marketed products. Beyond the observed AE of hypersensitivity and potential risk of helminthic parasitic infections common to the IL-5– and IL-5Rα–targeted therapies, major safety concerns have not been reported [20, 129,130,131]. The most recent ERS/ATS guidance suggests using anti‒IL-5 and anti‒IL-5Rα agents for severe uncontrolled adult eosinophilic asthma phenotypes, based on a meta-analysis of published efficacy and safety data, and acknowledges the adequate long-term safety profiles for these modalities thus far [4].
Eosinophils have been reported to promote tumor rejection or mitigate their growth based on indirect associations in humans and models of cancer progression in animals, raising potential concerns about the consequences of their therapeutic diminution [39, 69]. Attributing causality to a numerical imbalance in rare events such as malignancies or opportunistic infection is challenging in a clinical trial setting for several reasons. Observation times are typically short, statistical power is lacking, and AE reporting is potentially skewed (relative to the real-world setting) when patients are frequently and specifically asked about their health. Recent examples of this uncertainty involve the anti-asthma biologics omalizumab and reslizumab in which slight numerical imbalances in the overall frequencies of malignancies between active treatment and control arms in clinical trials resulted in precautionary language being required in certain product labels [26, 132]. This precaution remains in place for omalizumab in the USA despite the results of the 5-year observational cohort study EXCELS failing to demonstrate a meaningful difference in malignancies between the omalizumab (n = 5007) and non-omalizumab (n = 2829) cohorts [133]. The COLUMBA study reported a reassuring safety profile for 347 patients with severe asthma treated with open-label mepolizumab for an average of 3.5 years (maximum up to 4.5 years) total [92], with similar results reported for 1051 patients receiving reslizumab for up to 2 years [93]. The integrated analyses of patients with severe asthma (SIROCCO/CALIMA/BORA) and COPD (GALATHEA/TERRANOVA) demonstrated comparable occurrences of malignant neoplasms between benralizumab and placebo with no apparent change in risk during a second year of exposure for patients with asthma. The types and incidences of neoplasms that have developed during clinical trials would not be unexpected in the primarily middle-aged, adult populations studied [20, 134, 135].
Eosinophils may be involved in the immunologic response to infection. Occurrences of Herpes zoster infection have been reported with treatment with IL-5–targeted therapies. Our analysis demonstrated comparable incidences of Herpes zoster between benralizumab and placebo for patients with severe asthma and COPD. Herpes zoster has been reported post approval [136]. Cases of Herpes zoster have also been reported with mepolizumab, including during the initial clinical trials and post approval [137, 138]. Patients with known helminth infections were excluded from participation in registration clinical trials for benralizumab, mepolizumab, and reslizumab, and such infections are uncommon in countries where IL-5–targeted therapies have generally been trialed. Therefore, the safety of eosinophil-depleting therapies for patients traveling to endemic regions remains to be determined. To date, no data supporting increased susceptibility to other opportunistic infections have been reported [20].
As legitimate concerns around the potential risk of sustained eosinophil lowering/depletion still exist, continued pharmacovigilance is important. A subset of the original SIROCCO/CALIMA patients continue to be monitored as part of the ongoing MELTEMI (NCT02808819) safety extension, with estimated study completion in 2020. In addition, two large ongoing AstraZeneca-supported severe asthma registries (International Severe Asthma Registry [ISAR; http://isaregistries.org/] and US CHRONICLE [NCT03373045]) will assess certain safety measures (including incident malignancies) across the range of biologic and nonbiologic asthma treatments for patients with severe asthma, with an anticipated combined total of > 14,000 patients when fully recruited and observation times of at least 5 years.
6 Conclusions
Eosinophils have been associated with host protection against certain infections and malignancies primarily based on results from retrospective observational studies and nonclinical models of tumor progression, raising potential concerns in the medical community about the consequences of their therapeutic diminution. These observations conflict with the substantial clinical trial and real-world experience to date for eosinophil-lowering modalities, in general, with no evidence of specific differences in risk profile between the benralizumab mechanism of action and anti–IL-5 modalities. In clinical trials, anti–IL-5Rα therapy has been well-tolerated, with an overall AE profile similar to that with placebo in type and frequency. The integrated analyses of approximately 1600 patients with asthma (approximately 1000 of whom were exposed to benralizumab continuously for up to 2 years) and approximately 2700 patients with COPD (with exposure for approximately 1 year) suggests that eosinophil depletion by benralizumab treatment does not increase risk of infections or malignancies. The postmarketing experience to date supports this conclusion in the severe asthma population, for whom benralizumab is indicated. Rare cases of Herpes zoster have been reported, but the incidence is too small to determine an association with benralizumab. Helminthic infections were not reported in the clinical development program; however, the trials were generally not conducted in regions with a high prevalence of such infections, and patients with known helminth infections were excluded from participation in clinical trials [121]. Prospective, adequately powered, real-world studies should provide further insight into the potential risks of eosinophil-lowering therapies in the longer term.
References
Global Asthma Network. The global asthma report. 2018. http://www.globalasthmareport.org/Global%20Asthma%20Report%202018.pdf. Accessed 25 Oct 2019.
Chung KF, Wenzel SE, Brozek JL, Bush A, Castro M, Sterk PJ, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43:343–73.
Global Initiative for Asthma (GINA). Difficult-to-treat & severe asthma in adolescent and adult patients: diagnosis and management. 2019. Available at: ginasthma.org/wp-content/uploads/2019/04/GINA-Severe-asthma-Pocket-Guide-v2.0-wms-1.pdf. Accessed 16 Oct 2019.
Holguin F, Cardet JC, Chung KF, Diver S, Ferreira DS, Fitzpatrick A, et al. Management of severe asthma: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J. 2020;55. https://doi.org/10.1183/13993003.00588-2019.
Ravin KA, Loy M. The eosinophil in infection. Clin Rev Allergy Immunol. 2016;50:214–27.
Akuthota P, Wang H, Weller PF. Eosinophils as antigen-presenting cells in allergic upper airway disease. Curr Opin Allergy Clin Immunol. 2010;10:14–9.
Zhang JY, Wenzel SE. Tissue and BAL based biomarkers in asthma. Immunol Allergy Clin North Am. 2007;27(623–32):vi.
Price D, Wilson AM, Chisholm A, Rigazio A, Burden A, Thomas M, et al. Predicting frequent asthma exacerbations using blood eosinophil count and other patient data routinely available in clinical practice. J Asthma Allergy. 2016;9:1–12.
Talini D, Novelli F, Bacci E, Bartoli M, Cianchetti S, Costa F, et al. Sputum eosinophilia is a determinant of FEV1 decline in occupational asthma: results of an observational study. BMJ Open. 2015;5:e005748.
Pelaia C, Vatrella A, Busceti MT, Gallelli L, Terracciano R, Savino R, et al. Severe eosinophilic asthma: from the pathogenic role of interleukin-5 to the therapeutic action of mepolizumab. Drug Des Devel Ther. 2017;11:3137–44.
Schleich FN, Chevremont A, Paulus V, Henket M, Manise M, Seidel L, Louis R. Importance of concomitant local and systemic eosinophilia in uncontrolled asthma. Eur Respir J. 2014;44:97–108.
Green RH, Brightling CE, McKenna S, Hargadon B, Parker D, Bradding P, et al. Asthma exacerbations and sputum eosinophil counts: a randomised controlled trial. Lancet. 2002;360:1715–21.
Price DB, Rigazio A, Campbell JD, Bleecker ER, Corrigan CJ, Thomas M, et al. Blood eosinophil count and prospective annual asthma disease burden: a UK cohort study. Lancet Respir Med. 2015;3:849–58.
Marichal T, Mesnil C, Bureau F. Homeostatic eosinophils: characteristics and functions. Front Med (Lausanne). 2017;4:101.
Johansson MW. Eosinophil activation status in separate compartments and association with asthma. Front Med (Lausanne). 2017;4:75.
Qiu Y, Nguyen KD, Odegaard JI, Cui X, Tian X, Locksley RM, et al. Eosinophils and type 2 cytokine signaling in macrophages orchestrate development of functional beige fat. Cell. 2014;157:1292–308.
Jung Y, Wen T, Mingler MK, Caldwell JM, Wang YH, Chaplin DD, et al. IL-1beta in eosinophil-mediated small intestinal homeostasis and IgA production. Mucosal Immunol. 2015;8:930–42.
Lee JJ, Jacobsen EA, McGarry MP, Schleimer RP, Lee NA. Eosinophils in health and disease: the LIAR hypothesis. Clin Exp Allergy. 2010;40:563–75.
Takatsu K. Interleukin-5 and IL-5 receptor in health and diseases. Proc Jpn Acad Ser B Phys Biol Sci. 2011;87:463–85.
Roufosse F. Targeting the interleukin-5 pathway for treatment of eosinophilic conditions other than asthma. Front Med (Lausanne). 2018;5:49.
Palframan RT, Collins PD, Severs NJ, Rothery S, Williams TJ, Rankin SM. Mechanisms of acute eosinophil mobilization from the bone marrow stimulated by interleukin 5: the role of specific adhesion molecules and phosphatidylinositol 3-kinase. J Exp Med. 1998;188:1621–32.
Mukherjee M, Sehmi R, Nair P. Anti-IL5 therapy for asthma and beyond. World Allergy Organ J. 2014;7:32.
Ortega HG, Yancey SW, Mayer B, Gunsoy NB, Keene ON, Bleecker ER, et al. Severe eosinophilic asthma treated with mepolizumab stratified by baseline eosinophil thresholds: a secondary analysis of the DREAM and MENSA studies. Lancet Respir Med. 2016;4:549–56.
Castro M, Zangrilli J, Wechsler ME, Bateman ED, Brusselle GG, Bardin P, et al. Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: results from two multicentre, parallel, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet Respir Med. 2015;3:355–66.
GlaxoSmithKline LLC. Nucala® (mepolizumab) prescribing information. 2019. http://www.gsksource.com/pharma/content/dam/GlaxoSmithKline/US/en/Prescribing_Information/Nucala/pdf/NUCALA-PI-PIL.PDF. Accessed 16 Oct 2019.
Teva Respiratory LLC. Cinqair® (reslizumab) prescribing information. 2020. https://www.cinqair.com/globalassets/cinqair/prescribinginformation.pdf. Accessed 1 Apr 2020.
Kolbeck R, Kozhich A, Koike M, Peng L, Andersson CK, Damschroder MM, et al. MEDI-563, a humanized anti-IL-5 receptor alpha mAb with enhanced antibody-dependent cell-mediated cytotoxicity function. J Allergy Clin Immunol. 2010;125:1344–53.
Pham TH, Damera G, Newbold P, Ranade K. Reductions in eosinophil biomarkers by benralizumab in patients with asthma. Respir Med. 2016;111:21–9.
Kuang FL, Legrand F, Makiya M, Ware J, Wetzler L, Brown T, et al. Benralizumab for PDGFRA-negative hypereosinophilic syndrome. N Engl J Med. 2019;380:1336–46.
Singh D, Agusti A, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J. 2019;53:1900164. https://erj.ersjournals.com/content/53/5/1900164. Accessed 21 Mar 2020.
Singh D, Kolsum U, Brightling CE, Locantore N, Agusti A, Tal-Singer R. Eosinophilic inflammation in COPD: prevalence and clinical characteristics. Eur Respir J. 2014;44:1697–700.
Narendra DK, Hanania NA. Targeting IL-5 in COPD. Int J Chron Obstruct Pulmon Dis. 2019;14:1045–51.
Siva R, Green RH, Brightling CE, Shelley M, Hargadon B, McKenna S, et al. Eosinophilic airway inflammation and exacerbations of COPD: a randomised controlled trial. Eur Respir J. 2007;29:906–13.
Couillard S, Larivee P, Courteau J, Vanasse A. Eosinophils in COPD exacerbations are associated with increased readmissions. Chest. 2017;151:366–73.
Saetta M, Di Stefano A, Maestrelli P, Turato G, Ruggieri MP, Roggeri A, et al. Airway eosinophilia in chronic bronchitis during exacerbations. Am J Respir Crit Care Med. 1994;150:1646–52.
Singh D, Bafadhel M, Brightling CE, Sciurba FC, Curtis JL, Martinez FJ, et al. Blood Eosinophil Counts in Clinical Trials for Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2020;Mar 18. https://doi.org/10.1164/rccm.201912-2384pp(E-pub ahead of print).
Huang L, Appleton JA. Eosinophils in helminth infection: defenders and dupes. Trends Parasitol. 2016;32:798–807.
Phipps S, Lam CE, Mahalingam S, Newhouse M, Ramirez R, Rosenberg HF, et al. Eosinophils contribute to innate antiviral immunity and promote clearance of respiratory syncytial virus. Blood. 2007;110:1578–86.
Sakkal S, Miller S, Apostolopoulos V, Nurgali K. Eosinophils in cancer: favourable or unfavourable? Curr Med Chem. 2016;23:650–66.
Liu J, Lin PC, Zhou BP. Inflammation fuels tumor progress and metastasis. Curr Pharm Des. 2015;21:3032–40.
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–7.
Todoric J, Antonucci L, Karin M. Targeting inflammation in cancer prevention and therapy. Cancer Prev Res (Phila). 2016;9:895–905.
Vesterinen E, Pukkala E, Timonen T, Aromaa A. Cancer incidence among 78,000 asthmatic patients. Int J Epidemiol. 1993;22:976–82.
Boffetta P, Ye W, Boman G, Nyrén O. Lung cancer risk in a population-based cohort of patients hospitalized for asthma in Sweden. Eur Respir J. 2002;19:127–33.
Qu YL, Liu J, Zhang LX, Wu CM, Chu AJ, Wen BL, et al. Asthma and the risk of lung cancer: a meta-analysis. Oncotarget. 2017;8:11614–20.
Gonzalez-Perez A, Fernandez-Vidaurre C, Rueda A, Rivero E, Garcia Rodriguez LA. Cancer incidence in a general population of asthma patients. Pharmacoepidemiol Drug Saf. 2006;15:131–8.
Turner MC, Chen Y, Krewski D, Ghadirian P, Thun MJ, Calle EE. Cancer mortality among US men and women with asthma and hay fever. Am J Epidemiol. 2005;162:212–21.
Juhn YJ. Risks for infection in patients with asthma (or other atopic conditions): is asthma more than a chronic airway disease? J Allergy Clin Immunol. 2014;134:247–57 (quiz 58–9).
Yang M, Zhang Y, Chen H, Lin J, Zeng J, Xu Z. Inhaled corticosteroids and risk of upper respiratory tract infection in patients with asthma: a meta-analysis. Infection. 2019;47:377–85.
Capili CR, Hettinger A, Rigelman-Hedberg N, Fink L, Boyce T, Lahr B, et al. Increased risk of pertussis in patients with asthma. J Allergy Clin Immunol. 2012;129:957–63.
Juhn YJ, Frey D, Li X, Jacobson R. Streptococcus pyogenes upper respiratory infection and atopic conditions other than asthma: a retrospective cohort study. Prim Care Respir J. 2012;21:153–8.
Kim BS, Mehra S, Yawn B, Grose C, Tarrell R, Lahr B, et al. Increased risk of herpes zoster in children with asthma: a population-based case-control study. J Pediatr. 2013;163:816–21.
Kloepfer KM, Lee WM, Pappas TE, Kang TJ, Vrtis RF, Evans MD, et al. Detection of pathogenic bacteria during rhinovirus infection is associated with increased respiratory symptoms and asthma exacerbations. J Allergy Clin Immunol. 2014;133(1301–7):7.e1–3.
Busse WW, Gern JE. Asthma and infections: is the risk more profound than previously thought? J Allergy Clin Immunol. 2014;134:260–1.
Centers for Disease Control and Prevention. Pneumococcal vaccine timing for adults. http://www.cdc.gov/vaccines/vpd/pneumo/downloads/pneumo-vaccine-timing.pdf Accessed 9 Jan 2020.
Reichman H, Karo-Atar D, Munitz A. Emerging roles for eosinophils in the tumor microenvironment. Trends Cancer. 2016;2:664–75.
Fisher ER, Paik SM, Rockette H, Jones J, Caplan R, Fisher B. Prognostic significance of eosinophils and mast cells in rectal cancer: findings from the National Surgical Adjuvant Breast and Bowel Project (protocol R-01). Hum Pathol. 1989;20:159–63.
Nielsen HJ, Hansen U, Christensen IJ, Reimert CM, Brunner N, Moesgaard F. Independent prognostic value of eosinophil and mast cell infiltration in colorectal cancer tissue. J Pathol. 1999;189:487–95.
Jain M, Kasetty S, Sudheendra US, Tijare M, Khan S, Desai A. Assessment of tissue eosinophilia as a prognosticator in oral epithelial dysplasia and oral squamous cell carcinoma-an image analysis study. Patholog Res Int. 2014;2014:507512.
Fujii M, Yamashita T, Ishiguro R, Tashiro M, Kameyama K. Significance of epidermal growth factor receptor and tumor associated tissue eosinophilia in the prognosis of patients with nasopharyngeal carcinoma. Auris Nasus Larynx. 2002;29:175–81.
McNeel DG, Gardner TA, Higano CS, Kantoff PW, Small EJ, Wener MH, et al. A transient increase in eosinophils is associated with prolonged survival in men with metastatic castration-resistant prostate cancer who receive sipuleucel-T. Cancer Immunol Res. 2014;2:988–99.
Molin D. Bystander cells and prognosis in Hodgkin lymphoma. Review based on a doctoral thesis. Ups J Med Sci. 2004;109:179–228.
Samoszuk M. Eosinophils and human cancer. Histol Histopathol. 1997;12:807–12.
Keresztes K, Szollosi Z, Simon Z, Tarkanyi I, Nemes Z, Illes A. Retrospective analysis of the prognostic role of tissue eosinophil and mast cells in Hodgkin’s lymphoma. Pathol Oncol Res. 2007;13:237–42.
Wong TW, Kita H, Hanson CA, Walters DK, Arendt BK, Jelinek DF. Induction of malignant plasma cell proliferation by eosinophils. PLoS One. 2013;8(7):e70554.
Xie F, Liu LB, Shang WQ, Chang KK, Meng YH, Mei J, et al. The infiltration and functional regulation of eosinophils induced by TSLP promote the proliferation of cervical cancer cell. Cancer Lett. 2015;364:106–17.
van Driel WJ, Hogendoorn PC, Jansen FW, Zwinderman AH, Trimbos JB, Fleuren GJ. Tumor-associated eosinophilic infiltrate of cervical cancer is indicative for a less effective immune response. Hum Pathol. 1996;27:904–11.
Varricchi G, Galdiero MR, Loffredo S, Lucarini V, Marone G, Mattei F, et al. Eosinophils: the unsung heroes in cancer? Oncoimmunology. 2018;7:e1393134.
Gleich GJ, Klion AD, Lee JJ, Weller PF. The consequences of not having eosinophils. Allergy. 2013;68:829–35.
Beeson PB, Bass DA. The eosinophil. Major Probl Intern Med. 1977;14:1–269.
Nakahata T, Spicer SS, Leary AG, Ogawa M, Franklin W, Goetzl EJ. Circulating eosinophil colony-forming cells in pure eosinophil aplasia. Ann Intern Med. 1984;101:321–4.
Krantz SB, Kao V. Studies on red cell aplasia. I. Demonstration of a plasma inhibitor to heme synthesis and an antibody to erythroblast nuclei. Proc Natl Acad Sci USA. 1967;58:493–500.
Prazma CM, Bel EH, Price RG, Bradford ES, Albers FC, Yancey SW. Oral corticosteroid dose changes and impact on peripheral blood eosinophil counts in patients with severe eosinophilic asthma: a post hoc analysis. Respir Res. 2019;20:83.
Rice JB, White AG, Scarpati LM, Wan G, Nelson WW. Long-term systemic corticosteroid exposure: a systematic literature review. Clin Ther. 2017;39:2216–29.
Al Efraij K, Johnson KM, Wiebe D, Sadatsafavi M, FitzGerald JM. A systematic review of the adverse events and economic impact associated with oral corticosteroids in asthma. J Asthma. 2019;56:1334–46.
Yu C, Cantor AB, Yang H, Browne C, Wells RA, Fujiwara Y, et al. Targeted deletion of a high-affinity GATA-binding site in the GATA-1 promoter leads to selective loss of the eosinophil lineage in vivo. J Exp Med. 2002;195:1387–95.
Humbles AA, Lloyd CM, McMillan SJ, Friend DS, Xanthou G, McKenna EE, et al. A critical role for eosinophils in allergic airways remodeling. Science. 2004;305:1776–9.
Lee JJ, Dimina D, Macias MP, Ochkur SI, McGarry MP, O’Neill KR, et al. Defining a link with asthma in mice congenitally deficient in eosinophils. Science. 2004;305:1773–6.
Noffz G, Qin Z, Kopf M, Blankenstein T. Neutrophils but not eosinophils are involved in growth suppression of IL-4-secreting tumors. J Immunol. 1998;160:345–50.
Kruger-Krasagakes S, Li W, Richter G, Diamantstein T, Blankenstein T. Eosinophils infiltrating interleukin-5 gene-transfected tumors do not suppress tumor growth. Eur J Immunol. 1993;23:992–5.
Reichman H, Itan M, Rozenberg P, Yarmolovski T, Brazowski E, Varol C, et al. Activated eosinophils exert antitumorigenic activities in colorectal cancer. Cancer Immunol Res. 2019;7:388–400.
Mattes J, Hulett M, Xie W, Hogan S, Rothenberg ME, Foster P, et al. Immunotherapy of cytotoxic T cell-resistant tumors by T helper 2 cells: an eotaxin and STAT6-dependent process. J Exp Med. 2003;197:387–93.
Simson L, Ellyard JI, Dent LA, Matthaei KI, Rothenberg ME, Foster PS, et al. Regulation of carcinogenesis by IL-5 and CCL11: a potential role for eosinophils in tumor immune surveillance. J Immunol. 2007;178:4222–9.
Doris K, Karabela SP, Kairi CA, Simoes DC, Roussos C, Zakynthinos SG, et al. Allergic inflammation does not impact chemical-induced carcinogenesis in the lungs of mice. Respir Res. 2010;11:118.
Stathopoulos GT, Sherrill TP, Karabela SP, Goleniewska K, Kalomenidis I, Roussos C, et al. Host-derived interleukin-5 promotes adenocarcinoma-induced malignant pleural effusion. Am J Respir Crit Care Med. 2010;182:1273–81.
Zaynagetdinov R, Sherrill TP, Gleaves LA, McLoed AG, Saxon JA, Habermann AC, et al. Interleukin-5 facilitates lung metastasis by modulating the immune microenvironment. Cancer Res. 2015;75:1624–34.
Ikutani M, Yanagibashi T, Ogasawara M, Tsuneyama K, Yamamoto S, Hattori Y, et al. Identification of innate IL-5-producing cells and their role in lung eosinophil regulation and antitumor immunity. J Immunol. 2012;188:703–13. https://doi.org/10.4049/jimmunol.1101270.
Committee for Medicinal Products for Human Use (CHMP). Assessment report: Fasenra. 2017. http://www.ema.europa.eu/en/documents/assessment-report/fasenra-epar-public-assessment-report_en.pdf. Accessed 16 Oct 2019.
Center for Drug Evaluation and Research. Pharmacology/toxicology BLA review and evaluation of extractables and leachables from the container closure system (prefilled syringe). 2017. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2017/761070Orig1s000PharmR.pdf. Accessed 25 Oct 2019.
Food Drug Administration Center for Drugs Evaluation Research. Mepolizumab (Nucala) Medical Review. Biologics License Application (BLA). Review Completion Date: June 30, 2015. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2015/125526Orig1s000MedR.pdf. Accessed 9 Jan 2020.
Food Drug Administration Center for Drugs Evaluation Research. Reslizumab (Cinqair) Medical Review. Biologics License Application (BLA). Review Date: March 14, 2016. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2016/761033Orig1s000MedR.pdf. Accessed 9 Jan 2020.
Khatri S, Moore W, Gibson PG, Leigh R, Bourdin A, Maspero J, et al. Assessment of the long-term safety of mepolizumab and durability of clinical response in patients with severe eosinophilic asthma. J Allergy Clin Immunol. 2019;143:1742–51.
Murphy K, Jacobs J, Bjermer L, Fahrenholz JM, Shalit Y, Garin M, Zangrilli J, Castro M. Long-term safety and efficacy of reslizumab in patients with eosinophilic asthma. J Allergy Clin Immunol Pract. 2017;5:1572–81.
Bleecker ER, FitzGerald JM, Chanez P, Papi A, Weinstein SF, Barker P, et al. Efficacy and safety of benralizumab for patients with severe asthma uncontrolled with high-dosage inhaled corticosteroids and long-acting beta2-agonists (SIROCCO): a randomised, multicentre, placebo-controlled phase 3 trial. Lancet. 2016;388:2115–27.
FitzGerald JM, Bleecker ER, Nair P, Korn S, Ohta K, Lommatzsch M, et al. Benralizumab, an anti-interleukin-5 receptor alpha monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2016;388:2128–41.
Busse WW, Bleecker ER, FitzGerald JM, Ferguson GT, Barker P, Sproule S, et al. Long-term safety and efficacy of benralizumab in patients with severe, uncontrolled asthma: 1-year results from the BORA phase 3 extension trial. Lancet Respir Med. 2019;7:46–59.
Bass DA. Behavior of eosinophil leukocytes in acute inflammation. II. Eosinophil dynamics during acute inflammation. J Clin Invest. 1975;56:870–9.
Svensson L, Wenneras C. Human eosinophils selectively recognize and become activated by bacteria belonging to different taxonomic groups. Microbes Infect. 2005;7:720–8.
Lipkin WI. Eosinophil counts in bacteremia. Arch Intern Med. 1979;139:490–1.
Davido B, Makhloufi S, Matt M, Calin R, Senard O, Perronne C, et al. Changes in eosinophil count during bacterial infection: revisiting an old marker to assess the efficacy of antimicrobial therapy. Int J Infect Dis. 2017;61:62–6.
Shaaban H, Daniel S, Sison R, Slim J, Perez G. Eosinopenia: is it a good marker of sepsis in comparison to procalcitonin and C-reactive protein levels for patients admitted to a critical care unit in an urban hospital? J Crit Care. 2010;25:570–5.
Harrison AM, Bonville CA, Rosenberg HF, Domachowske JB. Respiratory syncytical virus-induced chemokine expression in the lower airways: eosinophil recruitment and degranulation. Am J Respir Crit Care Med. 1999;159:1918–24.
Percopo CM, Dyer KD, Ochkur SI, Luo JL, Fischer ER, Lee JJ, et al. Activated mouse eosinophils protect against lethal respiratory virus infection. Blood. 2014;123:743–52.
Domachowske JB, Dyer KD, Adams AG, Leto TL, Rosenberg HF. Eosinophil cationic protein/RNase 3 is another RNase A-family ribonuclease with direct antiviral activity. Nucleic Acids Res. 1998;26:3358–63.
Samarasinghe AE, Melo RCN, Duan S, LeMessurier KS, Liedmann S, Surman SL, et al. Eosinophils Promote Antiviral Immunity in Mice Infected with Influenza A Virus. J Immunol. 2017;198:3214–26.
Ramirez GA, Yacoub MR, Ripa M, Mannina D, Cariddi A, Saporiti N, et al. Eosinophils from physiology to disease: a comprehensive review. Biomed Res Int. 2018;2018:9095275.
Buys J, Wever R, van Stigt R, Ruitenberg EJ. The killing of newborn larvae of Trichinella spiralis by eosinophil peroxidase in vitro. Eur J Immunol. 1981;11:843–5.
Capron M, Torpier G, Capron A. In vitro killing of S. mansoni schistosomula by eosinophils from infected rats: role of cytophilic antibodies. J Immunol. 1979;123:2220–30.
Fabre V, Beiting DP, Bliss SK, Gebreselassie NG, Gagliardo LF, Lee NA, et al. Eosinophil deficiency compromises parasite survival in chronic nematode infection. J Immunol. 2009;182:1577–83.
Babayan SA, Read AF, Lawrence RA, Bain O, Allen JE. Filarial parasites develop faster and reproduce earlier in response to host immune effectors that determine filarial life expectancy. PLoS Biol. 2010;8:e1000525.
Chu VT, Beller A, Rausch S, Strandmark J, Zanker M, Arbach O, et al. Eosinophils promote generation and maintenance of immunoglobulin-A-expressing plasma cells and contribute to gut immune homeostasis. Immunity. 2014;40:582–93.
Hernandez JD, Li T, Rau C, Masuda MY, Madura JA, Jacobsen EA, Defilippis E. Decreased human adipose tissue-resident eosinophils in obese subjects is associated with increased insulin resistance. Diabetes. 2019;68(Suppl 1).
Kato M, Kephart GM, Talley NJ, Wagner JM, Sarr MG, Bonno M, et al. Eosinophil infiltration and degranulation in normal human tissue. Anat Rec (Hoboken). 1998;252:418–25.
Mesnil C, Raulier S, Paulissen G, Xiao X, Birrell MA, Pirottin D, et al. Lung-resident eosinophils represent a distinct regulatory eosinophil subset. J Clin Invest. 2016;126:3279–95.
Flood-Page PT, Menzies-Gow AN, Kay AB, Robinson DS. Eosinophil’s role remains uncertain as anti–interleukin-5 only partially depletes numbers in asthmatic airway. Am J Respir Crit Care Med. 2003;167:199–204.
Laviolette M, Gossage DL, Gauvreau G, Leigh R, Olivenstein R, Katial R, et al. Effects of benralizumab on airway eosinophils in asthmatic patients with sputum eosinophilia. J Allergy Clin Immunol. 2013;132:1086–96.
Nair P, Wenzel S, Rabe KF, Bourdin A, Lugogo NL, Kuna P, et al. Oral glucocorticoid-sparing effect of benralizumab in severe asthma. N Engl J Med. 2017;376:2448–58.
Chojnacki A, Wojcik K, Petri B, Aulakh G, Jacobsen EA, LeSuer WE, et al. Intravital imaging allows real-time characterization of tissue resident eosinophils. Commun Biol. 2019;2:181.
FASENRA™ (benralizumab) Periodic Benefit Risk Evaluation Report: through November 13, 2019 (DOF).
FitzGerald JM, Bleecker ER, Bourdin A, Busse WW, Ferguson GT, Brooks L, et al. Two-year integrated efficacy and safety analysis of benralizumab in severe asthma. J Asthma Allergy. 2019;12:401–13.
AstraZeneca. Fasenra™ (benralizumab) prescribing information. 2019. http://www.azpicentral.com/fasenra/fasenra.pdf#page=1. Accessed 16 Oct 2019.
AstraZeneca. Fasenra™ (benralizumab) summary of product characteristics. 2019. www.ema.europa.eu/en/documents/product-information/fasenra-epar-product-information_en.pdf. Accessed 16 Oct 2019.
Bourdin A, Shaw D, Menzies-Gow A, FitzGerald JM, Bleecker ER, Busse WW, et al. Two-year integrated steroid-sparing analysis and safety of benralizumab for severe asthma. J Asthma. 2019;26:1‒9. https://doi.org/10.1080/02770903.2019.1705333(E-pub ahead of print).
Criner GJ, Celli BR, Brightling CE, Agusti A, Papi A, Singh D, et al. Benralizumab for the prevention of COPD exacerbations. N Engl J Med. 2019;381:1023–34.
Padigel UM, Lee JJ, Nolan TJ, Schad GA, Abraham D. Eosinophils can function as antigen-presenting cells to induce primary and secondary immune responses to Strongyloides stercoralis. Infect Immun. 2006;74:3232–8.
Zeitlin PL, Leong M, Cole J, Mallory RM, Shih VH, Olsson RF, et al. Benralizumab does not impair antibody response to seasonal influenza vaccination in adolescent and young adult patients with moderate to severe asthma: results from the Phase IIIb ALIZE trial. J Asthma Allergy. 2018;11:181–92.
Kreindler J, Katial R, Barker P, Newbold P. Benralizumab Treatment is Not Associated with Oral Coritcosteroid-Like Increases in Weight and Blood Pressure. Ann Allergy Asthma Immunol. 2019;123(5):S39.
Roufosse FE, Kahn JE, Gleich GJ, Schwartz LB, Singh AD, Rosenwasser LJ, et al. Long-term safety of mepolizumab for the treatment of hypereosinophilic syndromes. J Allergy Clin Immunol. 2013;131(461–7):e1–5.
Teva Respiratory LLC. Cinqair® (reslizumab) summary of product characteristics. 2016. http://www.ema.europa.eu/en/documents/product-information/cinqaero-epar-product-information_en.pdf. Accessed 10 Jan 2020.
GlaxoSmithKline LLC. Nucala® (mepolizumab) summary of product characteristics. 2015. http://www.ema.europa.eu/en/documents/product-information/nucala-epar-product-information_en.pdf. Accessed 10 Jan 2020.
Bagnasco D, Ferrando M, Varricchi G, Puggioni F, Passalacqua G, Canonica GW. Anti-interleukin 5 (IL-5) and IL-5Ra biological drugs: efficacy, safety, and future perspectives in severe eosinophilic asthma. Front Med (Lausanne). 2017;4:135.
Genentech, Inc. Xolair (omalizumab) prescribing information. 2019. http://www.gene.com/download/pdf/xolair_prescribing.pdf. Accessed 10 Jan 2020.
Long A, Rahmaoui A, Rothman KJ, Guinan E, Eisner M, Bradley MS, et al. Incidence of malignancy in patients with moderate-to-severe asthma treated with or without omalizumab. J Allergy Clin Immunol. 2014;134:560–7.
Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, MacIntyre MF, et al. Wolfe C, Hamadeh RR. The global burden of cancer 2013. JAMA Oncol. 2015;1:505‒27.
Surveillance‚ Epidemiology‚ and End Results Program (SEER). Cancer statistics review (CSR) 1975-2016. 2019. seer.cancer.gov/csr/1975_2016/. Accessed 16 Oct 2019.
Mishra AK, Sahu KK, James A. Disseminated herpes zoster following treatment with benralizumab. Clin Respir J. 2019;13:189–91.
Haldar P, Brightling CE, Hargadon B, Gupta S, Monteiro W, Sousa A, et al. Mepolizumab and exacerbations of refractory eosinophilic asthma. N Engl J Med. 2009;360:973–84.
Benjamin MR, Bochner BS, Peters AT. Mepolizumab use: post-approval academic practice experience. Ann Allergy Asthma Immunol. 2018;121:126–8.
Acknowledgements
Writing and editing support was provided by Luke Burke, PhD (JK Associates, Inc., Conshohocken, PA, USA) and Michael A. Nissen, ELS (AstraZeneca, Gaithersburg, MD, USA). This support was funded by AstraZeneca.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
David J. Jackson has received advisory board and speaker fees from AstraZeneca. Stephanie Korn is a study investigator and has served on advisory boards for and received honoraria for symposia lectures from AstraZeneca. Sameer K. Mathur has received consulting and speaker fees from AstraZeneca. Peter Barker, Venkata G. Meka, Ubaldo J. Martin, and James G. Zangrilli are employees of AstraZeneca, the manufacturer of benralizumab, and each own stock in AstraZeneca.
Funding
The development of this review was funded by AstraZeneca.
Ethics
All patients enrolled in the trials used to generate the data reported here provided written informed consent at enrollment. All source studies were conducted in accordance with the principles of the Declaration of Helsinki and were consistent with the International Council for Harmonisation/Good Clinical Practice. Additional information is provided in the electronic supplementary material.
Data Availability
Data underlying the findings described in this manuscript may be requested in accordance with AstraZeneca’s data-sharing policy described at https://astrazenecagroup-dt.pharmacm.com/DT/Home.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Jackson, D.J., Korn, S., Mathur, S.K. et al. Safety of Eosinophil-Depleting Therapy for Severe, Eosinophilic Asthma: Focus on Benralizumab. Drug Saf 43, 409–425 (2020). https://doi.org/10.1007/s40264-020-00926-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-020-00926-3