Abstract
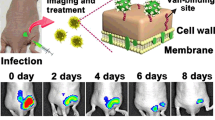
Staphylococcus aureus is one of the most frequent pathogens responsible for biofilm-associated infections. Among current clinical antibiotics, very few enable long-term successful treatment. Thus, it becomes necessary to better understand antibiotic failures and successes in treating infections in order to master the use of proper antibiotic therapies. In this context, we took benefit from a set of fluorescence spectroscopy and imaging methods, with the support of conventional microbiological tools to better understand the vancomycin–rifampin combination (in)efficiency against S. aureus biofilms. It was shown that both antibiotics interacted by forming a complex. This latter allowed a faster penetration of the drugs before dissociating from each other to interact with their respective biological targets. However, sufficiently high concentrations of free vancomycin should be maintained, either by increasing the vancomycin concentration or by applying repetitive doses of the two drugs, in order to eradicate rifampin-resistant mutants.
Similar content being viewed by others
References
F. D. Lowy, J. Clin. Invest., 2003, 111, 1265–1273.
C. E. Edmiston, A. J. McBain, C. Roberts, and D. Leaper, Adv. Exp. Med. Biol., 2015, 830, 47–67.
H.-C. Flemming, and J. Wingender, Nat. Rev. Microbiol., 2010, 8, 623–633.
P. A. Smith, and F. E. Romesberg, Nat. Chem. Biol., 2007, 3, 549–556.
H. Van Acker, P. Van Dijck, and T. Coenye, Trends Microbiol., 2014, 22, 326–333.
I. Levin-Reisman, I. Ronin, O. Gefen, I. Braniss, N. Shoresh, and N. Q. Balaban, Science, 2017, eaaj2191.
V. Kostenko, H. Ceri, and R. J. Martinuzzi, FEMS Immunol. Med. Microbiol., 2007, 51, 277–288.
K. L. LaPlante, and S. Woodmansee, Antimicrob. Agents Chemother., 2009, 53, 3880–3886.
S. Deresinski, Clin. Infect. Dis., 2009, 49, 1072–1079.
H.-J. Tang, C.-C. Chen, K.-C. Cheng, K.-Y. Wu, Y.-C. Lin, C.-C. Zhang, T.-C. Weng, W.-L. Yu, Y.-H. Chiu, H.-S. Toh, S.-R. Chiang, B. A. Su, W.-C. Ko, and Y.-C. Chuang, Antimicrob. Agents Chemother., 2013, 57, 5717–5720.
O. Cirioni, F. Mocchegiani, R. Ghiselli, C. Silvestri, E. Gabrielli, E. Marchionni, F. Orlando, D. Nicolini, A. Risaliti, and A. Giacometti, Eur. J. Vasc. Endovasc. Surg., 2010, 40, 817–822.
S. M. Jones, M. Morgan, T. J. Humphrey, and H. Lappin-Scott, Lancet, 2001, 357, 40–41.
D. C. Bean, and S. M. Wigmore, mBio, 2015, 6, e00120–e00115.
G. N. Forrest, and K. Tamura, Clin. Microbiol. Rev., 2010, 23, 14–34.
W. Zimmerli, R. Frei, A. F. Widmer, and Z. Rajacic, J. Antimicrob. Chemother., 1994, 33, 959–967.
W. Wehrli, Rev. Infect. Dis., 1983, 5, S407–S411.
J. C. Barna, and D. H. Williams, Annu. Rev. Microbiol., 1984, 38, 339–357.
J. A. Niska, J. H. Shahbazian, R. I. Ramos, K. P. Francis, N. M. Bernthal, and L. S. Miller, Antimicrob. Agents Chemother., 2013, 57, 5080–5086.
D. C. Coraça-Huber, M. Fille, J. Hausdorfer, K. Pfaller, and M. Nogler, J. Appl. Microbiol., 2012, 112, 1235–1243.
F. D. Lowy, D. S. Chang, and P. R. Lash, Antimicrob. Agents Chemother., 1983, 23, 932–934.
P. Vergidis, M. S. Rouse, G. Euba, M. J. Karau, S. M. Schmidt, J. N. Mandrekar, J. M. Steckelberg, and R. Patel, Antimicrob. Agents Chemother., 2011, 55, 1182–1186.
C. Watanakunakorn, and J. C. Guerriero, Antimicrob. Agents Chemother., 1981, 19, 1089–1091.
A. H. Salem, W. F. Elkhatib, and A. M. Noreddin, J. Pharm. Pharmacol., 2011, 63, 73–79.
G. L. Simon, R. H. Smith, and M. A. Sande, Rev. Infect. Dis., 1983, 5, Suppl. 3, S507–S508.
S. Tremblay, T. T. Y. Lau, and M. H. H. Ensom, Ann. Pharmacother., 2013, 47, 1045–1054.
D. J. Riedel, E. Weekes, and G. N. Forrest, Antimicrob. Agents Chemother., 2008, 52, 2463–2467.
A. S. van der Horst, S. Medda, E. Ledbetter, A. Liu, P. Weinhold, D. J. Del Gaizo, and L. Dahners, J. Orthop. Res., 2015, 33, 1320–1326.
S. Daddi Oubekka, R. Briandet, M.-P. Fontaine-Aupart, and K. Steenkeste, Antimicrob. Agents Chemother., 2012, 56, 3349–3358.
R. Boudjemaa, R. Briandet, M. Revest, C. Jacqueline, J. Caillon, M.-P. Fontaine-Aupart, and K. Steenkeste, Antimicrob. Agents Chemother., 2016, 60, 4983–4990.
P. S. Stewart, J. Bacteriol., 2003, 185, 1485–1491.
S. Daddi Oubekka, R. Briandet, F. Waharte, M.-P. Fontaine-Aupart, and K. Steenkeste, in Proc. SPIE 8087, Clinical and Biomedical Spectroscopy and Imaging II, 80871I, ed. N. Ramanujam and J. Popp, 2011, pp. 80871I–1–80871I–7.
F. Waharte, K. Steenkeste, R. Briandet, and M.-P. Fontaine-Aupart, Appl. Environ. Microbiol., 2010, 76, 5860–5869.
A. Tupin, M. Gualtieri, F. Roquet-Banères, Z. Morichaud, K. Brodolin, and J.-P. Leonetti, Int. J. Antimicrob. Agents, 2010, 35, 519–523.
N. Høiby, T. Bjarnsholt, M. Givskov, S. Molin, and O. Ciofu, Int. J. Antimicrob. Agents, 2010, 35, 322–332.
Acknowledgments
The authors thank the Centre de Photonique Biomédicale (CPBM) of the Centre Laser de l’Université Paris-Sud (CLUPS/LUMAT FR2764, Orsay, France) for the confocal microscope and L2 microbiology facilities, and Rachel Méallet-Renault for the spectrofluorimeter facilities at the Ecole Normale Supérieure (ENS Cachan).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boudjemaa, R., Briandet, R., Fontaine-Aupart, MP. et al. How do fluorescence spectroscopy and multimodal fluorescence imaging help to dissect the enhanced efficiency of the vancomycin–rifampin combination against Staphylococcus aureus infections?. Photochem Photobiol Sci 16, 1391–1399 (2017). https://doi.org/10.1039/c7pp00079k
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1039/c7pp00079k